Welcome back to Healthy Innovations! 👋
This week I wanted to explore the impact of remote patient monitoring (RPM) on clinical trials. New technology now means that patients can be part of cutting-edge clinical trials without ever leaving their living room. No more weekly hospital commutes, no hours spent in waiting rooms, no interrupting daily life for medical research.
Today, this is the reality for patients across conditions from Parkinson’s to diabetes to heart failure. Using everyday devices - smartphones, wearables, and smart pill bottles - patients can now join trials from anywhere, while researchers gather richer, real-world data than ever before.
So let’s dive in!
Fact-based news without bias awaits. Make 1440 your choice today.
Overwhelmed by biased news? Cut through the clutter and get straight facts with your daily 1440 digest. From politics to sports, join millions who start their day informed.
The current clinical trial system leaves patients behind
For decades, clinical trials have struggled with an accessibility problem that’s bigger than many realise. In the US alone, most people live more than two hours from a research centre. That distance instantly excludes millions who can’t afford the time, cost or disruption of constant travel.
Even for those who can take part, the burden is high: arranging childcare, taking unpaid leave, and spending hours in hospital waiting rooms. One study found that 64% of cancer trial participants incurred unexpected non-medical, trial-related expenses, with 51% spending over $600 per month and 21% exceeding $1,500 per month.
Meanwhile, the data collected only reflects short, artificial snapshots of health - a blood pressure reading under perfect clinic conditions tells you little about a stressful work day or a restless night at home.
Many patients drop out before trials end, which compromises the data and slows down research. And those who do complete trials often come from the same narrow demographic - skewing results and leaving real-world questions unanswered.
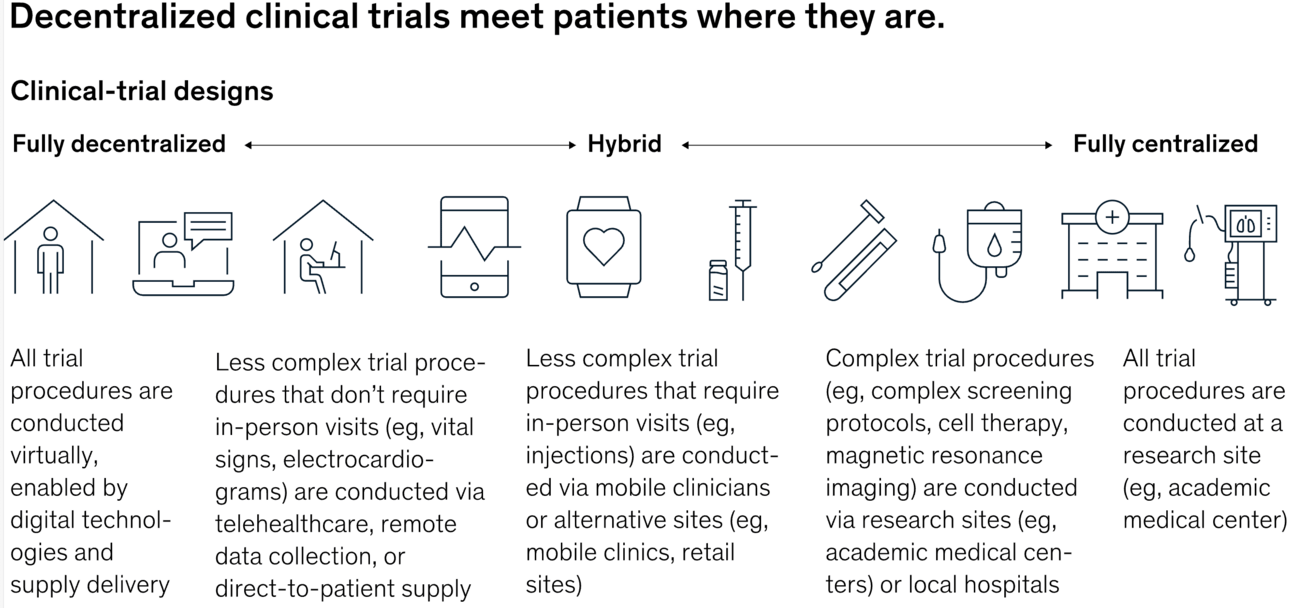
There is a better way - decentralized clinical trials (DCTs, or virtual clinical trials) that utilize remote patient monitoring.
Impact of Covid-19 pandemic
The COVID-19 pandemic rapidly accelerated the adoption of decentralized clinical trials, as traditional site-based research became challenging due to restrictions and safety concerns. Sponsors and regulators quickly turned to remote methods like telemedicine, electronic consent, and at-home monitoring to maintain research continuity. This shift not only kept trials running during lockdowns but also improved accessibility, patient engagement, and flexibility. As a result, DCTs have become a transformative and lasting feature of modern clinical research.
Bringing the hospital home
Instead of forcing patients to adapt to rigid trial schedules, DCTs let research adapt to patients’ everyday lives.
A patient with a rare neurodegenerative disease can take part in a study from the comfort of their own living room. A student with asthma can help answer important medical questions from their dorm room.
DCTs use a mix of standalone and connected devices that patients are instructed how to use. These include blood pressure monitors, pulse oximeters, smart pill bottles, wearables, smartphone apps, biological sampling kits, telehealth platforms as well as simple patient journals. A lot of work has gone into ensuring these tools meet the needs of a wide range of patients with varying levels of health literacy.
Continuous data: the real breakthrough
What makes remote patient monitoring so powerful is not just the gadgets - it’s the quality and depth of the evidence they generate via real-time monitoring. Traditional trials are like taking a few photos and trying to guess the full story. Remote patient monitoring is like watching the whole film, frame by frame.
Look at diabetes research: where once doctors relied on occasional blood tests, continuous glucose monitors now show exactly how blood sugar behaves during meals, stress, exercise and sleep. It’s a far clearer, more realistic picture.
Smartphones and wearables also pick up subtle changes that humans can’t easily detect. Voice patterns, gait shifts, or reaction times can reveal how well a treatment is working, sometimes weeks before traditional assessments would show a difference.
Safety also improves. Researchers don’t have to wait for scheduled appointments to spot a problem - they see warning signs in real time and can intervene immediately. And smart devices can confirm whether patients are actually taking their medication, avoiding one of the biggest blind spots in trials.
Better trials, faster answers
The evidence is clear, DCTs demonstrate:
✅ Higher retention rates: Studies show retention rates can increase significantly in trials using remote tools. A decentralized approach for a Phase 4 breast cancer trial led to a 96% patient retention rate, representing an estimated 30% improvement over traditional site-based oncology trials, where retention rates typically hover around 70%.
✅ Broader reach: DCTs can include rural patients and underrepresented groups, improving diversity and scientific validity. Critical for rare and ultra-rare diseases as patients scattered across continents can finally participate in meaningful research.
✅ Faster results: By removing geographic barriers, trials hit recruitment targets quicker - speeding up the pipeline for new treatments.
✅ Cost-effectiveness: A single day delay to a clinical trial can cost a pharmaceutical company up to $40,000 in direct daily clinical trial costs, so speeding up recruitment and keeping retention rates up, will help keep costs down.
The hybrid future
While not every aspect of a trial can happen at home, hybrid models are becoming the norm. Complex scans and procedures still happen at clinics. Routine check-ins, symptom diaries, and safety monitoring run remotely. This balance keeps patients engaged and trials efficient, without losing human connection when it matters most.
Remaining challenges
Challenges remain. Not everyone has the latest smartphone or reliable internet. Some older patients or people with disabilities may need extra help. Researchers must prove that consumer devices are as trustworthy as traditional tests. And global privacy rules can still complicate multi-country trials.
But the direction is clear: people want trials that are more patient-friendly, more representative, and more rooted in everyday reality.
Why this matters
The big promise of remote patient monitoring is simple: it brings medical research closer to real life, speeding up discoveries and getting better treatments to patients sooner.
For people with serious diseases, every month shaved off a trial timeline means hope arrives sooner. For scientists, it means clearer answers faster - and fewer wasted resources chasing dead ends.
When the living room becomes the lab, everyone wins.
Innovation highlights
🏥 Lost in translation. An ER in Australia is developing a multilingual AI chatbot that speaks fluent "my head hurts" in dozens of languages. This digital translator helps triage nurses understand patients who can't explain their symptoms in English, preventing dangerous mix-ups where chest pain gets mistaken for heartburn due to language barriers. The AI processes symptoms in real-time, ensuring everyone gets properly prioritized - regardless of their vocabulary skills.
⚡ Electric age detection. Researchers have discovered that aged cells have unique electrical signatures that can be detected using electric fields. This groundbreaking technique can distinguish between young and old cells by their distinct electrical properties, potentially revolutionizing how we identify and target senescent cells. The non-invasive method could lead to new therapies for age-related diseases by helping scientists zap away troublesome aged cells that contribute to aging.
🧬 Genetic wake-up call. Scientists have discovered a clever new gene therapy trick: instead of adding new genes, they're playing genetic matchmaker by deleting DNA segments to bring sleepy genes closer to their "on switches." Using CRISPR-like molecular scissors, researchers successfully reactivated dormant genes that could help treat sickle cell disease and beta-thalassemia - proving sometimes the best cure is already hiding in our cells, just waiting for the right introduction.
Cool tool
📌 Milanote is a unique visual organization app I've used for years. Think of it as a digital pinboard where you can drag and drop notes, images, videos, links, and files anywhere you want - perfect for visual thinkers who find traditional list-based tools limiting.
Since it syncs seamlessly across iPhone, iPad, Android, Mac, and PC, your boards are always accessible. Though originally built for creative professionals, it's fantastic for project planning, research organization, and brainstorming. You can even use it for your next home reno project!
Company to watch
🎤 Ultraspeaking is transforming communication training through game-based learning that helps people master public speaking. Founded by Tristan and Michael - who achieved the fastest-ever path to the World Championship of Public Speaking finals - this company uses interactive games and hands-on practice to help participants reach a "flow state" during high-pressure speaking.
While traditional courses rely on passive lectures, Ultraspeaking throws participants into active practice through live virtual sessions, expert coaching, and a supportive global community. Their method helps people bring their natural, relaxed communication style into professional settings. Featured as a case study in the Wall Street Journal bestseller Ultralearning, their accelerated approach has transformed how people handle both formal presentations and everyday professional conversations.
Weird and wonderful
🩸 One-of-a-kind blood. French scientists have discovered the world's 48th blood type, dubbed "Gwada negative," in a Guadeloupean woman during routine pre-surgery tests. After 14 years of research using advanced DNA sequencing, she remains the only known carrier of this ultra-rare blood group. Talk about being truly unique - this woman is literally one in eight billion!
Thank you for reading the Healthy Innovations newsletter!
Keep an eye out for next week’s issue, where I will highlight the healthcare innovations you need to know about.
Have a great week!
Alison ✨
P.S. Join over 500 healthcare leaders who get these insights delivered straight to their inbox! Healthy Innovations is read weekly by executives from AstraZeneca, GSK, Vertex, Roche, and leading healthcare startups, agencies, and investors. Subscribe now to stay ahead of industry trends!